We aim to touch a billion lives with our best-in-class services.


Did you know that you can easily submit your claims online?
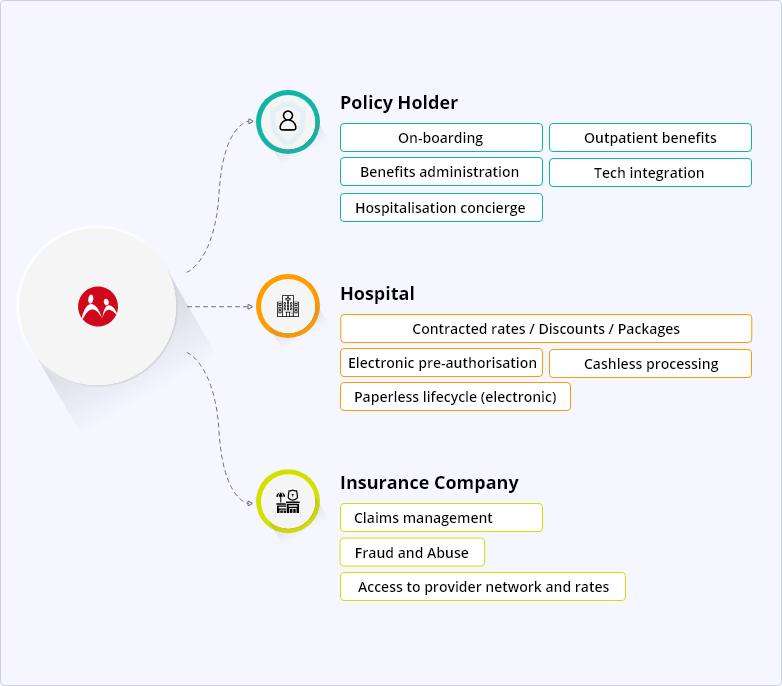
Read moreMedi Assist partners with group accounts (employers) to administer their employee health insurance plans, in India and overseas through Mayfair We Care. Additionally, we partner with Insurers to administer health insurance plans for retail customers (individual insurance Policyholders) and publicly funded health schemes (Government Schemes) as well.
Our differentiators
Competitive rates/contracts
Creative solutions that deliver value from their benefits investment and improve health.
Simplified program delivery
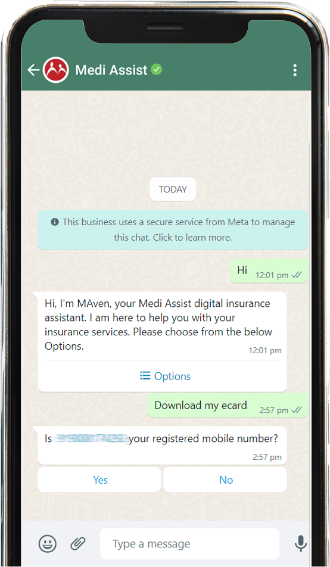
For a unified, engaging employee experience, we offer a range of digital platforms designed to improve the employee benefits experience.
Global healthcare network
Access to healthcare services via hospitals, healthcare providers and medical centers in 141 countries
Optimized benefits
We don't believe in a one-size-fits-all solution. Our approach delivers real-world solutions using Medi Assist-proprietary tools.
Prevention of fraud and abuse
We use features like electronic KYC, Two-factor authentication for claim registration to protect member data from fraudulent activities online.
Medi Assist's role in the health insurance ecosystem
Our Footprint as of H1 - FY 24
Claim intimation

Claim intimation
Members can intimate Medi Assist for an upcoming admission to hospital or at the time of discharge from the hospital. Intimation allows us to serve our members better and prepare in advance.
e-Card

e-Card
An e-Card identifies a member and dependents covered under a health insurance policy and helps the member know of their choice of third-party administrator (TPA).
e-Cashless

e-Cashless
When the members have a planned hospitalization need, they can avail the benefit of this offering. They can get their hospitalization pre-authorized prior to the actual date of admission, simply using the member portal/app.
Locating a hospital

Locating a hospital
Medi Assist members can access an exhaustive list of approved hospitals on our app (MAven) or portal (mediassist.in). Members can then select a network hospital of choice.
Reimbursement claim submission
Reimbursement claim submission
Members can electronically upload relevant hospital documents (claim file) on our app or portal to initiate a reimbursement claim settlement. Paper copies of the claim documents can follow wherever insurers need the original paper documents for verification.

Always by your side, making every experience easy and smooth
General helpline: 0120 693 7372
Senior citizen helpline: 1800 419 9493